Poor sleep and heart disease are more closely connected than most people realize. In our increasingly demanding world, cutting back on sleep often feels like a necessity. But new findings are sounding the alarm: just three nights of inadequate or fragmented sleep can substantially elevate your risk of developing heart disease. While long-term sleep deprivation has been linked to cardiovascular issues for years, emerging evidence indicates that harm can begin within mere days.
A comprehensive study from Columbia University, backed by data from the American Heart Association (AHA) and international research including the UK Biobank cohort, reveals that short-term sleep disturbances can elevate blood pressure, disrupt heart rate patterns, and increase inflammatory markers—even in otherwise healthy individuals. This underscores the evolving view of sleep as not just a wellness choice but a fundamental pillar of cardiovascular health.
Why Poor Sleep and Heart Disease Are Closely Linked
Sleep is often underestimated, yet its quality directly influences cardiovascular resilience. Beyond total sleep time, the continuity and depth of sleep play critical roles in the body’s nightly restoration processes.
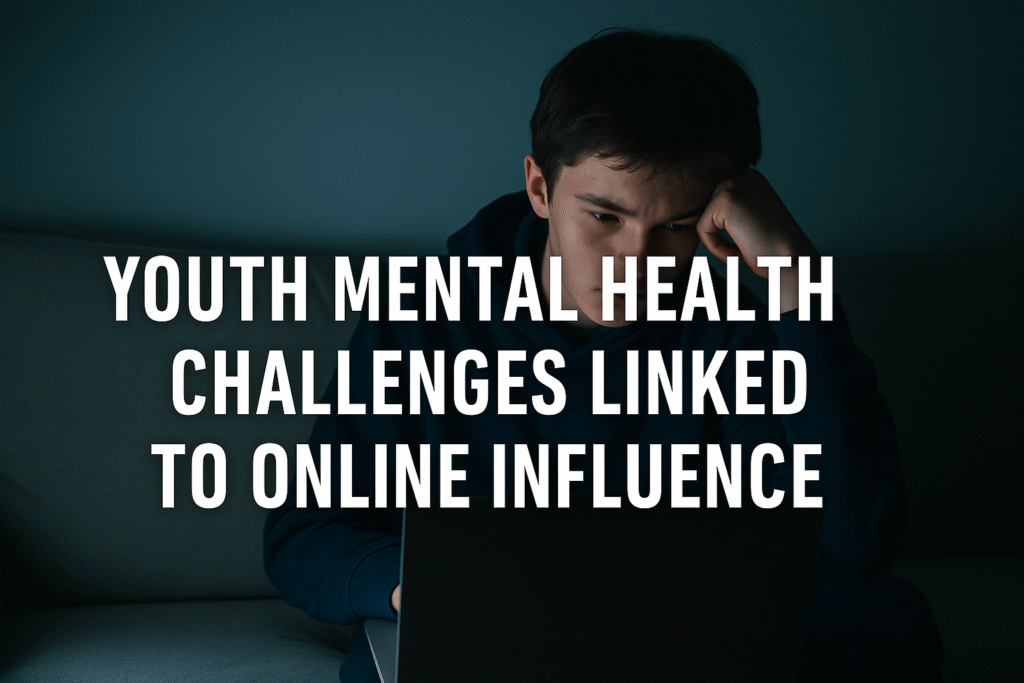
During high-quality sleep, the body:
- Lowers blood pressure and heart rate, allowing vascular repair
- Suppresses cortisol and other stress hormones
- Regulates glucose metabolism and inflammatory pathways
Disrupted sleep—caused by stress, digital exposure, inconsistent schedules, or disorders like sleep apnea—prevents these restorative functions. The result: heightened sympathetic nervous system activity, increased nighttime blood pressure, and persistent low-grade inflammation. These are recognized precursors to hypertension, atherosclerosis, and cardiac arrhythmias.
In a 2024 study published in Hypertension (AHA), adults subjected to three nights of restricted sleep (4 hours per night) experienced significant increases in systolic blood pressure and inflammatory biomarkers such as interleukin-6 and C-reactive protein. These inflammatory agents are known to damage vascular linings and promote the formation of arterial plaques.
Fragmented Sleep: The Hidden Culprit
It’s not only about sleep duration—frequent awakenings during the night can be equally harmful. Fragmented sleep reduces the amount of time spent in restorative deep sleep and REM stages, leading to physiological stress. A 2023 meta-analysis in Sleep Health found that individuals with sleep fragmentation had a 27% higher risk of coronary artery disease compared to those with uninterrupted sleep.
Real-world scenarios—such as new parents, shift workers, and frequent travelers—illustrate how easily sleep patterns can be disrupted. Unfortunately, the body doesn’t fully adapt to these irregularities, and cardiovascular strain accumulates silently over time.
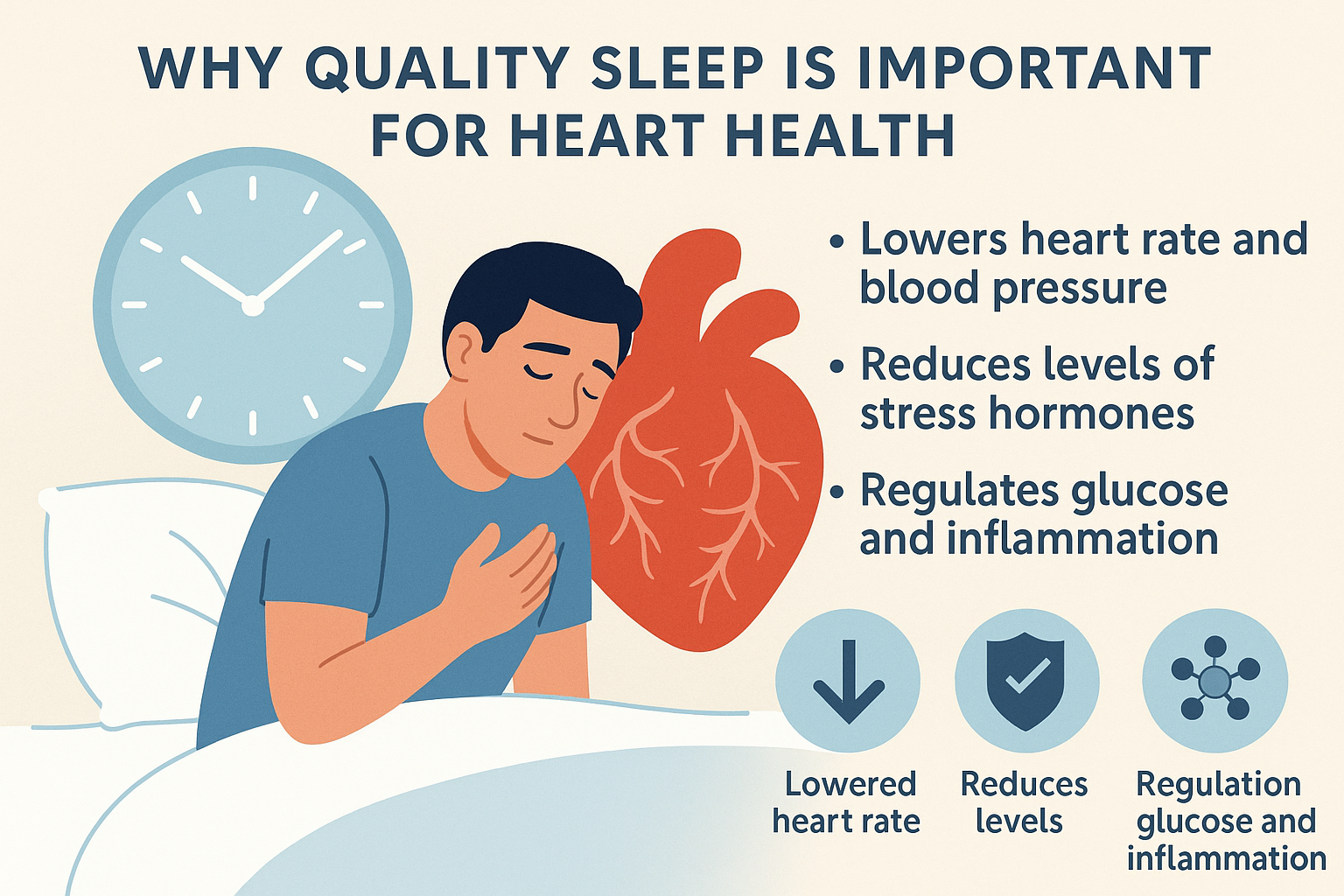
The Ideal Bedtime for a Healthy Heart
When you sleep may be as critical as how long you sleep. According to a 2021 study published in the European Heart Journal – Digital Health, individuals who consistently went to bed between 10:00 PM and 11:00 PM had the lowest incidence of cardiovascular events.
This bedtime window aligns with the body’s circadian rhythm—our internal clock that governs hormonal release, blood pressure regulation, and core body temperature. Deviation from this rhythm can:
- Disrupt melatonin synthesis, crucial for nighttime blood pressure regulation
- Affect heart rate variability (HRV), an indicator of autonomic balance
- Impair deep sleep stages that support endothelial function and tissue repair
The UK Biobank study (n=88,000) found that those who fell asleep after midnight faced a 12–25% increased risk of heart disease, independent of sleep duration or other lifestyle factors.
International Context: How Sleep Patterns Differ
Globally, cultures with strong sleep routines—like certain Mediterranean or East Asian populations—show lower rates of heart disease despite other risk factors. In contrast, industrialized nations with high rates of shift work and screen time before bed (e.g., the U.S., U.K., and Japan) see disproportionally higher levels of sleep disruption and related cardiovascular issues.
Sleep vs. Traditional Cardiovascular Risk Factors
Mounting research suggests that short-term poor sleep can rival more traditional cardiovascular risks. The physiological toll of even a few nights of disrupted sleep resembles the effects of smoking, high cholesterol, or sedentary behavior:
| Risk Factor | Short-Term Impact | Long-Term Effect |
|---|---|---|
| Smoking | Triggers inflammation and clot formation | Promotes atherosclerosis and heart attack |
| High cholesterol | Accelerates arterial plaque buildup | Increases risk of stroke and coronary events |
| Inactivity | Reduces cardiac output and metabolic health | Leads to obesity and type 2 diabetes |
| Poor sleep (3 nights) | Elevates blood pressure, increases IL-6/CRP | Raises risk of heart attack and stroke |
This comparison highlights that sleep disturbances—often dismissed as harmless—can act synergistically with other risk factors, accelerating cardiovascular decline.
Protecting Your Heart Through Better Sleep
Fortunately, the damage caused by short-term poor sleep can be reversed with consistent, restorative habits. Cardiologists and sleep researchers recommend:
- Maintaining a consistent bedtime (ideally 10–11 PM)
- Avoiding screens, caffeine, and alcohol before bed
- Creating a dark, quiet sleep environment
- Using sleep-tracking apps or devices to monitor quality
Natural sleep supplements can support these efforts when used responsibly. For instance:
NiteHush Pro contains calming botanicals and amino acids that promote deeper sleep cycles without causing morning drowsiness.
Sonus Complete, though designed for tinnitus support, may benefit those experiencing mental hyperactivity or nighttime disruptions, fostering a quieter mind at bedtime.
A 2024 AHA study found that participants who improved sleep hygiene for just two weeks saw significant drops in C-reactive protein and nighttime blood pressure—both strong indicators of cardiovascular health. Moreover, improvements in heart rate variability were observed, suggesting enhanced autonomic regulation.
Main Takeaways (Bullet Points)
- Just three nights of poor sleep can increase inflammation and blood pressure, key drivers of heart disease.
- Sleep quality and timing are as important as duration for cardiovascular protection.
- Fragmented sleep disrupts deep restorative stages, increasing heart risk.
- Going to bed between 10–11 PM aligns with natural circadian rhythms linked to lower heart risk.
- The effects of short-term sleep loss can mimic those of major lifestyle risks like smoking.
- Cultural habits and shift work patterns influence cardiovascular sleep risk globally.
- Lifestyle improvements and sleep supplements can help reverse early cardiovascular strain.
Further Reading
To explore the broader impact de hábitos de vida na saúde do coração, leia nosso artigo:
👉 Synthetic Food Dyes Ban 2026 – U.S. Regulation Timeline
Fontes
- American Heart Association. (2024). Hypertension Journal. https://www.ahajournals.org/journal/hyp
- UK Biobank Study, European Heart Journal – Digital Health (2021). https://academic.oup.com/ehjdh
- Columbia University Medical Center. https://www.cuimc.columbia.edu/
- Sleep Health Journal. Meta-analysis on Sleep Fragmentation (2023). https://www.sleephealthjournal.org